Clinical depression
A major problem with long term depression is that our mind gets habituated to it and it becomes our daily experience. The mind begins to habitually reinforce the depression.
The best way out of depression is to stop responding to life in a depressed manner.
The depressed person feels disconnected from life and the most important thing that we can do is to try to connect with life in all areas. This is the path out of depression. To be consciously connecting with every area of life.
It is difficult to begin with but like any habit we must try and by trying then sooner or later we will be connected with life. This requires conscious effort and honesty with ourself and others.
It your birth right to be here and you are allowed to be here and connected with life.
Coming out of long term and habitual depression is a journey that has been likened to walking down a long dark corridor because it takes time for the brain to start thinking clearly again and for us to achieve and maintain a healthy, balanced lifestyle.
Clinical depression is a state of sadness or melancholia that has advanced to the point of being disruptive to an individual's social functioning and/or activities of daily living. The diagnosis may be applied when an individual meets a sufficient number of the symptomatic criteria for the depression spectrum as suggested in the DSM-IV-TR or ICD-9/10. An individual is often seen to suffer from what is termed a "clinical depression" without fully meeting the various criteria advanced for a specific diagnosis on the depression spectrum. There is an ongoing debate regarding the relative importance of genetic or environmental factors, or gross brain problems versus psychosocial functioning.
Although a mood characterized by sadness is often colloquially referred to as depression, clinical depression is something more than just a temporary state of sadness. Symptoms lasting two weeks or longer, and of a severity that begins to interfere with typical social functioning and/or activities of daily living, are considered to constitute clinical depression.
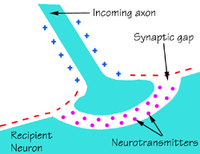
Clinical depression was originally considered to be a "chemical imbalance" in transmitters in the brain, a theory based on observations made in the 1950s of the effects of reserpine and isoniazid in altering monoamine neurotransmitter levels and affecting depressive symptoms [1] . Subsequent antidepressants have also been found to alter monoamine levels, particularly of serotonin and noradrenaline [2] . Despite a growing body of evidence suggesting otherwise, it is still a commonly held belief that depression is only a chemical imbalance. This idea is often promoted in pharmaceutical advertising, and perpetuated in everyday discussions. Despite this reliance on "common wisdom", recent research and commentary has begun to address depression as an issue broader than this.
Clinical depression affects about 16%[3] of the population on at least one occasion in their lives. The mean age of onset, from a number of studies, is in the late 20s. About twice as many females as males report or receive treatment for clinical depression, though this imbalance is shrinking over the course of recent history; this difference seems to completely disappear after the age of 50 - 55, when most females have passed the end of menopause. Clinical depression is currently the leading cause of disability in the US as well as other countries, and is expected to become the second leading cause of disability worldwide (after heart disease) by the year 2020, according to the World Health Organization[4] .
On a historical note, the modern idea of depression appears similar to the much older concept of melancholia. The name melancholia derives from 'black bile', one of the 'four humours' postulated by Galen.
The Ebers papyrus (ca 1550 BC) contains a short description of clinical depression. Though full of incantations and foul applications meant to turn away disease-causing demons and other superstition, it also evinces a long tradition of empirical practice and observation.
Contents
|
Signs and symptoms
According to the DSM-IV-TR criteria for diagnosing a major depressive disorder (see also: DSM cautionary statement) one of the following two required elements need to be present:
- Depressed mood, or
- Loss of interest or pleasure.
It is sufficient to have either of these symptoms in conjunction with four of a list of other symptoms. These include:
- Feelings of overwhelming sadness or fear, or the seeming inability to feel emotion.
- A decrease in the amount of pleasure derived from what were previously pleasurable activities.
- Changing appetite and marked weight gain or weight loss.
- Disturbed sleep patterns, such as insomnia, loss of REM sleep, or excessive sleep.
- Changes in activity levels, such as restlessness or a slowing of movement.
- Fatigue, either/both mental and physical.
- Feelings of guilt, helplessness, hopelessness, anxiety, and/or fear.
- A decrease in self-esteem.
- Trouble concentrating or making decisions, or a generalized slowing and obtunding of cognition.
- Self-harm or ruminating on self-harm.
- Ruminating on death and/or suicide.
- Reduced memory.
Depression in children is not as obvious as it is in adults. Here are some symptoms that children might display:
- Loss of appetite.
- Sleep problems, such as recurrent nightmares.
- Learning or memory problems where none existed before.
- Significant behavioural changes; such as withdrawal, social isolation and aggression.
An additional indicator could be the excessive use of drugs or alcohol. Depressed adolescents are at particular risk of further destructive behaviors, such as eating disorders and self-harm.
One of the most widely used instruments for measuring depression severity is the Beck Depression Inventory, a 21 question multiple choice survey.
It is hard for people who have not experienced clinical depression, either personally or by regular exposure to people suffering it, to understand its emotional impact and severity, interpreting it instead as being similar to "having the blues" or "feeling down". As the list of symptoms above indicates, clinical depression is a serious, potentially lethal systemic disorder characterized by interlocking physical, affective, and cognitive symptoms which have consequences for function and survival well beyond sad or painful feelings.
Types of depression
Major Depression
Major Depression, or, more properly, 'Major Depressive Disorder' (MDD) is characterized by a severely depressed mood that persists for at least two weeks, and is generally recognized to contain an organic (chemical) component. Major Depressive Disorder is specified as either "a single episode" or "recurrent", as periods of depression may occur as discrete events or as recurrent over the lifespan.
Diagnosticians recognize several sub-types of Major Depressive Disorder.
- Catatonic Features Specification - Catatonia is characterized by motoric immobility evidenced by catalepsy or stupor. This MDD sub-type may also manifest excessive, non-prompted motor activity (akathesia), extreme negativism and/or mutism, and peculiarities in movement, including stereotypical movements, prominent mannerisms, and/or prominent grimacing. There may also be evidence of echolalia or echopraxia.
- Melancholic Features Specification - Melancholia is characterized by a loss of pleasure (anhedonia) in most or all activities, a failure of reactivity to pleasurable stimuli, a quality of depressed mood more pronounced than that of grief or loss, a worsening of symptoms in the morning hours, early morning waking, psychomotor retardation, anorexia (excessive weight loss, not to be confused with Anorexia Nervosa), and/or excessive guilt.
- Atypical Features Specification Atypicality is characterized by mood reactivity (paradoxical anhedonia) and positivity, significant weight gain or increased appetite, excessive sleep or somnolence (hypersomnia), leaden paralysis, and/or significant social impairment as a consequence of hyper-sensitivity to perceived interpersonal rejection.
- Psychotic Features Specification presents with hallucinations or delusions that are either mood-congruent (content coincident with depressive themes) or non-mood-congruent (content not coincident with depressive themes). It is clinically more common to encounter a delusional system as an adjunct to depression than to encounter hallucinations, whether visual or auditory.
Other Categories of Depression
Dysthymia is a long-term, mild depression that lasts for a minimum two years. By definition the symptoms are not as severe as with Major Depression, although those with Dysthymia are vulnerable to co-occurring episodes of Major Depression. This disorder often begins in adolescence, and crosses the lifespan.
Bipolar I Disorder is an episodic illness in which moods may cycle between mania and depression. In the US, Bipolar Disorder was previously referred to as "Manic Depression". This term is no longer favored by the medical community as not all Bipolar individuals will present depressive symptoms. "Manic Depression" is still often used in the non-medical community.
Bipolar II Disorder is an episodic illness that is defined primarily by depression, but evidences episodes of hypomania.
The role of anxiety in depression
Anxiety
The different types of Depression and Anxiety are classified separately by the DSM-IV-TR, with the exception of hypomania, which is included under the Bipolar Disorder category. Despite the different categories, depression and anxiety can indeed be co-occurring (occurring together, independently, and without mood congruence), or co-morbid (occurring together, with overlapping symptoms, and with mood congruence). In an effort to bridge the gap between the DSM-IV-TR categories and what clinicians actually encounter, experts such as Herman Van Praag of the Maastricht University have proposed ideas like anxiety/aggression-driven depression [citation needed]. This idea, and others like it, refers to an anxiety/depression spectrum for these two disorders, which differs from the mainstream perspective of discreet diagnostic categories.
While there is no specific diagnostic category for the co-morbidity of depression and anxiety in the DSM or ICD, the National Comorbidity Survey (US) reports that some 58 percent of those with major depression also suffer from lifetime anxiety citation. Supporting of this finding, two widely accepted clinical colloquiallisms include:
-
- agitated depression - referring to a state of depression that presents as anxiety, that includes akathisia, suicide, insomnia (not early morning wakefulness), non-clinical (meaning “doesn’t meet the standard for formal diagnosis”) and non-specific panic, and a general sense of dread.
-
- akathitic depression - referring to a state of depression that presents as anxiety, suicide, and includes akathisia, but does not include symptoms of panic.
It is also clear that even mild anxiety symptoms can have a major impact on the course of a depressive illness, and the co-mingling of any anxiety symptoms with the primary depression is important to consider. A pilot study by Ellen Frank PhD, et. al., at the University of Pittsburgh found that depressed or bipolar patients with lifetime panic symptoms experienced significant delays in their weeks to remission. [citation needed] These patients also had higher levels of residual impairment, or the ability to get back into the swing of things. On a similar note, Robert Sapolsky PhD of Stanford University, and others, also argue that the relationship between stress, anxiety, and depression could be measured and demonstrated biologically. [citation needed]. To that point, a study by Heim and Nemeroff, et. al., of Emory University found that depressed and anxious women with a history of childhood abuse recorded higher heart rates and the stress hormone ACTH when subjected to a stressful situation.
Hypomania
Hypomania, as the name suggests, is a state of mind and/or behavior that is "below" (hypo) mania. In other words, a person in a hypomanic state will often display behavior that has all the earmarks of a full-blown mania (marked elevation of mood that is characterized by euphoria, overactivity, disinhibition, impulsivity, a decreased need for sleep, hypersexuality, etc.), but these symptoms, while disruptive and seemingly out of character, will not be so pronounced as to be considered a diagnosibly manic episode.
Another important point is that hypomania is a diagnostic category that includes both anxiety and depression. It often presents as a state of anxiety that occurs within the context of a clinical depression. Patients in a hypomanic state often describe a sense of extreme generalized and/or specific anxiety, re-recurring panic attacks, night terrors, guilt, and agency (as it pertains to co-dependence and counter-dependence). All of this happens while they are in a state retarded or somnolent depression. This is the type of depression where a person is lethargic and unable to move through life. The terms “retarded” and “somnolent” are shorthand for states of depression that include lethargy, hypersomnia, a lack of motivation, a collapse of ADLs (activities of daily living), and social withdrawal. This is similar to the shorthand used to describe an "agitated" or "akathitic" depression.
In considering the hypomania-depression connection, one other distinction should be made. That is the differentiation among anxiety, panic, and stress. Anxiety is a physiological state that is caused by the sympathetic nervous system. Anxiety does not need an outside influence to occur. Panic is related to the "fight or flight" mechanism. It is a reaction, induced by an outside stimulus, and is a product of the sympathetic nervous system, and the cerebral cortex. More plainly, panic is an anxiety state that we are thinking about. Finally, stress is a psycho-social reaction, influenced by how a person filters non-threatening external events. This filtering is based on his/her own ideas, assumptions, and expectations. Taken together, these ideas, assumptions, and expectations are referred to as social constructionism.
On a final note, researchers at the University of California, San Diego under the guidance of Hagop Akiskal MD, have found convincing evidence for the co-occurrence of hypomanic symptoms associated with a diagnosis of depression where the diagnosis does not meet criteria for a Bipolar diagnosis.[citation needed] Symptoms under consideration, such as irritability, mis-directed anger, and compulsivity, also may not present sufficiently to be considered a hypomanic episode, as described by a Bipolar II Disorder. As noted in the Frank study [citation needed] mentioned above, this particular course of the disease, with the breakthrough of anxiety, may have a significant impact on the overall course of the depression.
This idea of co-occurring anxiety and depresion is supported in a study by Giovanni Cassano MD of the University of Pisa, and his collaborators on the Spectrum Project, who found a correlation between lifetime hypomanic and manic symptoms, and the severity of the depression.[citation needed]
- “The presence of a significant number of manic/hypomanic items in patients with recurrent unipolar depression seems to challenge the traditional unipolar-bipolar dichotomy...”
These authors, along with many other researchers,[citation needed] argue in support of a revision of the approach to psychiatric diagnosis into what is being referred to the mood spectrum, so as to “...[make] more accurate diagnostic evaluation[s].” This approach, although controversial, has begun to be given consideration by many behavioral health professionals.
Causes of depression
No specific cause for depression has been identified, but there are a number of factors believed to be involved.
- Heredity – The tendency to develop depression may be inherited; there is some evidence that this disorder may run in families. [citation needed]
- Physiology – There may be changes or imbalances in chemicals which transmit information in the brain, called neurotransmitters. Many modern antidepressant drugs attempt to increase levels of certain neurotransmitters, like serotonin and norepinephrine. While the causal relationship is unclear, it is known that antidepressant medications do relieve certain symptoms of depression, although critics point out that the relationship between serotonin, SSRIs, and depression is usually greatly oversimplified when presented to the public (see here). Seasonal affective disorder (SAD) is a type of depressive disorder that occurs in the winter when daylight hours are short. It is believed that the body's production of melatonin, which is produced at increased levels in the dark, plays a major part in the onset of SAD, and that many sufferers respond well to bright light therapy, also known as phototherapy. High levels of Omega-6 fatty acids in the brain have also been linked to depression.
- Psychological factors – Low self-esteem and self-defeating or distorted thinking are connected with depression. While it is not clear which is the cause and which is the effect, it is known that sufferers who are able to make corrections to their thinking patterns can show improved mood and self-esteem. Psychological factors include the complex development of one's personality and how one has learned to cope with external environmental factors, such as stress.
- Early experiences – Events such as the death of a parent, abandonment or rejection, neglect, chronic illness, and severe physical, psychological, or sexual abuse can also increase the likelihood of depression later in life. Post-traumatic stress disorder (PTSD) includes depression as one of its major symptoms.
- Life experiences – Job loss, financial difficulties, long periods of unemployment, the loss of a spouse or other family member, divorce or the end of a committed relationship, or other traumatic events may trigger depression. Long-term stress, at home, work or school, can also be involved.
- Medical conditions – Certain illnesses including cardiovascular pathologies[5] , hepatitis, mononucleosis, hypothyroidism, and organic brain damage caused by either degenerative conditions such as Parkinson disease or by traumatic blunt force injury may contribute to depression, as may certain prescription drugs such as birth control pills and steroids.
- Diet – The increase in depression in industrialised societies has been linked to diet; in particular to reduced levels of omega-3 fatty acids in intensively farmed food and processed foods[6] . This link has been, at least partly, validated by studies using dietry supplements in schools[7] and by a double blind test in a prison.
- Alcohol and other drugs – Alcohol can have a negative effect on mood, and misuse or abuse of alcohol, benzodiazepine-based tranquillizers and sleeping medications can all play a major role in the length and severity of depression. The link between frequent cannabis use and depression is also widely documented, although the direction of causality remains in question.[citation needed]
- Postpartum depression (also known as postnatal depression) – About ten percent of new mothers experience some form of depression after childbirth.[citation needed] When it occurs, the onset is typically within three months after delivery, and it may last for several months. About two new mothers out of a thousand have depression so severe it includes hallucinations or delusions.
- Living with a depressed person – Those living with someone suffering from depression experience increased anxiety, and life disruption, increasing the possibility of also becoming depressed.
- Social environment – Evolutionary theory suggests that depression is a protective mechanism: if an individual is involved in a lengthy fight for dominance of a social group and is clearly losing, depression causes the individual to back down and accept the submissive role. In doing so, the individual is protected from unnecessary harm. In this way, depression maintains the social hierarchy.
- Other evolutionary theories – Another evolutionary theory is that the cognitive response that produces modern day depression evolved as a mechanism that allows people to assess whether they are in pursuit of an unreachable goal. Still others claim that depression can be linked to perfectionism. People that accept satisfactory outcomes in lieu of "the best" outcome tend to lead happier lives. [citation needed]
Treatment
Treatment of depression varies broadly, and is different for each individual. Various types and combinations of treatments may have to be tried. There are two primary modes of treatment, typically employed in conjunction with one another: medication and psychotherapy. A third treatment, electro-convulsive therapy (ECT) may be used where chemical treatment fails.
Other alternative treatments used for depression include exercise and the use of vitamins, herbs, or other nutritional supplements.
The effectiveness of treatment often depends on factors such as the amount of optimism and hope the sufferer is able to maintain, the control s/he has over stressors, the severity of symptoms, the amount of time the sufferer has been depressed, the results of previous treatments, and the degree of support of family, friends, and significant others.
While treatment is generally effective, there are some cases where the condition fails to respond. Treatment-resistant depression requires a full assessment which may lead to the addition of psychotherapy, higher medication doses, changes of medication or combination therapy, a trial of ECT/electroshock, or even a change in the diagnosis with subsequent treatment changes. Although this process helps many, some people's symptoms continue unabated.
In emergency situations with suicidal persons, psychiatric hospitalization is used simply to keep suicidal people safe until they cease to be dangers to themselves. Another treatment program is partial hospitalization, in which the patient sleeps at home but spends the day, either five or seven days a week, in a psychiatric hospital setting in intense treatment. This treatment usually involves group therapy, individual therapy, psychopharmacology, and academics (in child and adolescent programs).
Medication
Medication which relieves the symptoms of depression has been available for several decades. These drugs are listed in order of historical development. Typical first line therapy for depression is the use of an SSRI type drug, such as sertraline (Zoloft).
Monoamine oxidase inhibitors (MAOIs) such as Nardil may be used if other antidepressant medications are ineffective. Because there are potenially fatal interactions between this class of medication and certain foods and drugs, they are rarely prescribed anymore. A new MAOI has recently been introduced. Moclobemide (Manerix), known as a reversible inhibitor of monoamine oxidase A (RIMA), follows a very specific chemical pathway and does not require a special diet.
Tricyclic antidepressants are the oldest, and include such medications as amitriptyline and desipramine. They are used less commonly now, due to side-effects which may include increased heart rate, drowsiness, dry mouth, and memory impairment. Most importantly, they have a high potential to be lethal in moderate overdose. The reason why tricyclic antidepressants are still used is their high potency, especially in severe cases of clinical depression.
Selective serotonin reuptake inhibitors (SSRIs) comprise the current standard family of antidepressants. It is thought that one cause of depression is that an inadequate amount of serotonin, a chemical which the brain uses to transmit signals between nerve cells, is produced. These drugs are said to work by preventing the reabsorption of serotonin by the nerve cell, thus maintaining the levels the brain needs to function effectively, although two researchers recently demonstrated that this is a marketing technique rather than a scientific portrayal of how the drugs actually work. [8]. Recent research indicates that these drugs may interact with transcription factors known as "clock genes"[9] that may be important for the addictive properties of drugs of abuse and possibly in obesity[10][11].
This family of drugs includes fluoxetine (Prozac), paroxetine (Paxil), escitalopram (Lexapro), and sertraline (Zoloft). These antidepressants typically have fewer adverse side effects than the tricyclics or the MAOIs, though such effects as drowsiness, dry mouth, and decreased ability to function sexually may occur.
Norepinephrine reuptake inhibitors such as reboxetine (Edronax) act via norepinephrine (Also known as noradrenaline). NeRIs are thought to have a positive effect on concentration and motivation in particular.
Serotonin-norepinephrine reuptake inhibitors (SNRIs) such as venlafaxine (Effexor) and duloxetine (Cymbalta) are a newer form of anti-depressant which work both on noradrenaline and on serotonin. They typically have similar side-effects to the SSRIs although there may be a withdrawal syndrome on discontinuation which may require a tapering of the dose.
On 28 February 2006, the United States Food and Drug Administration approved Emsam, a transdermal MAOI patch developed by the British company Somerset Pharmaceuticals, to be marketed in the U.S. by Bristol-Myers Squibb [12].
Dietary supplements
5-HTP supplements are claimed to provide more raw material to the body's natural serotonin production process. There is a reasonable indication that 5-HTP may not be effective for those who haven't already responded well to an SSRI.
S-adenosyl methionine (SAM-e) is a derivative of the amino acid methionine that is found throughout the human body, where it acts as a methyl donor and participates in other biochemical reactions. It is available as a prescription antidepressant in Europe, and an over-the-counter dietary supplement in the United States. Clinical trials have shown SAM-e to be as effective as standard antidepressant medication, with many fewer side effects.[13] ,[14] Its mode of action is unknown.
Omega-3 fatty acids (found naturally in oily fish, flax seeds, hemp seeds, walnuts, canola oil etc.) have also been found to be effective while used as a dietary supplement (although only fish-based omega-3 fatty acids have shown anti-depressant efficacity) [15].
Magnesium has gathered some attention [16][17].
Essential nutrients
A healthy diet is essential for removing depression. Many symptoms of depression are directly linked to malnutrition.
Zinc, an optimal level of which has had an antidepressant effect in studies [18][19].
Augmentor drugs
Some antidepressants have been found to work more effectively in some patients when used in combination with another drug. Such "augmentor" drugs include tryptophan (Tryptan) and buspirone (Buspar).
Tranquillizers and sedatives, typically the benzodiazepines, may be prescribed to ease anxiety and promote sleep. Because of their high potential for fostering dependence, these medications are intended only for short-term or occasional use. Medications are often employed not for their primary function, but to exploit what are normally side effects. Quetiapine fumarate (Seroquel) is designed primarily to treat schizophrenia and bipolar disorder, but a frequently-reported side-effect is somnolence. Hence, this non-addictive drug can be used in place of an addictive anti-anxiety agent such as clonazepam (Klonopin, Rivotril).
Antipsychotics such as risperidone (Risperdal) and olanzapine (Zyprexa), and Quetiapine (Seroquel) are prescribed as mood stabilizers and are also effective in treating anxiety. Antipsychotics (typical or atypical) may be also prescribed in an attempt to augment an antidepressant, to make antidepressant blood concentration higher, or to relieve psychotic or paranoid symptoms often accompanying clinical depression. However, they may have serious side effects, particularly at high doses, which may include blurred vision, muscle spasms, restlessness, tardive dyskinesia, and weight gain.
Antidepressants by their nature are stimulants. Anti-anxiety medications by their nature are depressants. Close medical supervision is critical to proper treatment if a subject is presenting both illnesses as the medications tend to work against each other.
Lithium remains the standard treatment for bipolar disorder, and is often used in conjunction with other medications, depending upon whether mania or depression is being treated. Lithium's potential side effects include thirst, tremors, light-headedness, and nausea or diarrhea. Some of the anticonvulsants such as carbamazepine (Tegretol), sodium valproate (Epilim), and lamotrigine (Lamictal) are also used as mood stabilisers, particularly in bipolar disorder.
Failure to take medication, or failure to take it as prescribed, is one of the major causes of relapse. Should one feel a change or discontinuation of medication is necessary, it is critical that this be done in consultation with a doctor.
Psychotherapy
In psychotherapy, or counselling, one receives assistance in understanding and resolving problems which may be contributing to depression. This may be done individually or with a group, and is conducted by health professionals such as psychiatrists, psychologists, social workers, or psychiatric nurses. It is important to enquire about both the therapist's training and approach; a very close bond often forms between practitioner and client, and it is important that the client feel understood by the clinician.
Counsellors can help a person make changes in thinking patterns, deal with relationship issues, detect and deal with relapses, and understand the factors that contribute to depression.
There are many therapeutic approaches, but all are aimed at improving an individual's personal and interpersonal functioning. Cognitive therapy, also known as Cognitive Behaviour Therapy, focuses on how people think about themselves and their relationships to the world. It works to counteract negative thought patterns and enhance self-esteem. Therapy can be used to help a person develop or improve interpersonal skills in order to allow them to communicate more effectively and reduce stress. Narrative therapy gives attention to each individual's "dominant story" by means of therapeutic conversations which also may involve exploring "unhelpful" ideas and how they came to prominence. Behavioral therapy is based on the assumption that behaviors are learned. This type of therapy attempts to teach individuals new and healthier types of behaviours. Supportive therapy encourages people to discuss their problems and provides them with emotional support. The focus is on sharing information, ideas, and strategies for coping with daily life. Family systems therapy helps people live together more harmoniously and undo patterns of destructive behaviour.
Transcranial magnetic stimulation
Repetitive transcranial magnetic stimulation (rTMS) is currently under study as a possible treatment for depression. Initially designed as a tool for physiological studies of the brain, this technique shows promise as a means of alleviating depression. In this therapy, a powerful magnetic field is used to stimulate the left prefrontal cortex, an area of the brain which typically shows abnormal activity in depressed individuals.
rTMS has been proposed as an alternative to ECT that would have fewer side effects. No sedation is required, and the only reported side effects are a slight headache in some patients, and facial muscle contraction during treatment. However clear evidence that it is an effective treatment is still awaited.[20]
Recent work in Poland has suggested that weak, variable magnetic fields may offer relief from depression in those that have been unresponsive to medication. However, some of the existing work has been questioned with claims that the effect is not as significant once environmental conditions are controlled for.
Vagus nerve stimulation
Vagus nerve stimulation therapy is a treatment used since 1997 to control seizures in epileptic patients and has recently been approved for treating resistant cases of clinical depression. The VNS device is implanted in a patient's chest with wires that connect it to the vagus nerve, which it stimulates to reach a region of the brain associated with moods. The device delivers controlled electrical doses to the vagus nerve at regular intervals.
Electroconvulsive therapy
Electroconvulsive therapy (ECT), also known as electroshock or electroshock therapy employs short bursts of a controlled current of electricity (this is typically fixed at 0.9 ampere) into the brain to induce a brief, artificial seizure while the patient is under general anaesthesia.
ECT has acquired a fearsome reputation, in part, from its use as a tool of repression in the former USSR, and its fictional depiction in films such as One Flew Over the Cuckoo's Nest, but remains a common treatment where other means of treatment have failed, or where the use of drugs is unacceptable (such as in pregnancy). Also, in contrast to "direct" electroshock of years ago, most countries now only allow ECT to be administered under anaesthesia. In a typical regimen of treatment, a patient receives three treatments per week over three or four weeks. Repeat sessions may be required. Short-term memory loss, disorientation and headache are very common side effects. In some cases, permanent memory loss has occurred, but detailed neuropsychological testing in clinical studies have not been able to prove permanent effects on memory. ECT offers the benefit of a very fast response, however, this response has been shown not to last unless either maintenance electroshock or maintenance medications are used. While antidepressants usually take around a month to take effect, the results of ECT have been shown to be much faster. For this reason, it is the treatment of choice in emergency circumstances (for example in catatonic depression where the patient has ceased oral intake of fluid or nutrients).
There remains much controversy over electroshock. Advocacy groups and scientific critics, such as Dr Peter Breggin[21], call for restrictions on its use or complete abolishment. Like all forms of psychiatric treatment, electroshock can be given without a patient's consent, but this is subject to legal conditions dependent on the jurisdiction.
Other methods of treatment
Light therapy
Bright light (both sunlight and artificial light) is shown to be effective in seasonal affective disorder, and sometimes may be effective in other types of depression, especially atypical depression or depression with "seasonal phenotype" (overeating, oversleeping, weight gain, apathy).
Important note: an antidepressant effect is caused by stimulation of the retina by the visible light, not by the ultra-violet portion. Thus, it is not necessary (and may be even dangerous in some cases) to get sunburn. It can be enough just to walk at daytime or to take light therapy using a light box. However, recent discoveries of the existence and importance of the third kind of photoreceptor in our eyes, the intrinsically photosensitive retinal ganglion cells(ipRGC)- critical to human chronobiology - strongly suggest that bluish light is more helpful, and manufacturers are beginning to respond to this.
Exercise
It is widely believed that physical activity and exercise helps depressive patients and promotes quicker and better relief from depression. It is also thought to help antidepressants and psychotherapy to work better and faster. It can be difficult to find the motivation to exercise if the depression is severe, but sufferers should be encouraged to take part in some form of regularly-scheduled physical activity if possible. A workout need not be strenuous; many find walking, for example, to be of great help. Exercise produces higher levels of chemicals in the brain, notably dopamine, serotonin, and norepinephrine. In general this leads to improvements in mood, which is effective in countering depression.
Note that prior to beginning an exercise regime, it is wise to consult a doctor. He or she can establish whether a person possesses any health problems that could rule out some types of exercise.
Meditation
Meditation is increasingly seen as a useful treatment for depression. The current professional opinion of meditation is that it represents at least a complementary method of treating depression, a view that has been clearly underscored by the Mayo Clinic. Since the late 1990s, much research has been carried out to determine how meditation affects the brain (for more information see the main article on meditation). While the effects on the mind are somewhat complex, they are often quite positive, encouraging a calm, reflective and rational state of mind which can be of great help against depression. It's notable that while many religions actively encourage/use meditative practice, it is not necessary to be a member of any faith to partake in meditation.
Old methods
Insulin shock treatment is an old and currently mostly abandoned treatment of severe depressions, psychoses, catatonic states and other mental disorders. It consists of induction of hypoglycemic coma by intravenous infusion of insulin. The treatment is potentially unsafe and can be lethal in some cases (about 1% of patients undergoing insulin coma), even with proper monitoring. That was the main reason why it was abandoned from current medical practice. In contrast, ECT is considered to be very safe.
Nevertheless, insulin shock therapy is still officially used in Russia and some other countries, and can be administered to a very treatment-resistant patient under his written consent in many Western countries.
Atropinic shock therapy, also known as atropinic coma therapy, is an old and currently rarely-used method. It consists of induction of atropinic coma by rapid intravenous infusion of atropine.
The atropinic shock treatment is considered relatively safe but the problem with its administration is that it requires prolonged coma (4-5 hours), careful monitoring and preparation, and it has many unpleasant side effects, like blurred vision due to atropine. Thus it is rarely used now. But it can be used under written consent in Western countries in some very treatment-resistant cases, and is still officially used in Russia and some other countries.
Relapse
Relapse is more likely if treatment has not resulted in the full remission of symptoms.4 In fact, current guidelines for antidepressant use recommend 4 to 6 months of continuing treatment following symptom resolution to prevent relapse of depression.
Combined evidence from many randomized controlled trials indicates that continuing antidepressant medications after recovery substantially reduces (halves) the chances of relapse. This preventative effect probably lasts for at least the first 36 months of use.[22]
Some anecdotal evidence exists to suggest that chronic disease is accompanied by relapses after prolonged treatment with antidepressants (Tachyphylaxis). Psychiatric texts suggest that physicians respond to this by increasing dosage, complementing the medication with a different class, or changing the medication class entirely. The reason for relapse in these cases is as poorly understood as the change in brain physiology induced by the medications themselves. Possible reasons may include ageing of the brain or worsening of the condition. Most SSRI psychiatric medications were developed for short term use (a year or less), but are widely prescribed for indefinite periods.[23]
See also
- Beck Depression Inventory
- Bipolar disorder
- Chemical imbalance theory
- Cyclothymia
- Dysthymia
- Hamilton Depression Rating Scale
- Hypoadrenia (also covers 'adrenal exhaustion', sometimes called 'adrenal fatigue')
- Learned helplessness
- List of people who have suffered from depression
- Mania
- Maslow's hierarchy of needs
- Seasonal affective disorder (SAD)
- Stress
Books
Books by psychologists/psychiatrists
- Beck, A. T., Rush, A. J., Shaw, B. F., Emery, G. (1987). Cognitive therapy of depression. New York: Guilford.
- Burns, David D. (1999). Feeling Good : The New Mood Therapy. Avon.
- Klein, D. F., & Wender, P. H. (1993). Understanding depression: A complete guide to its diagnosis and treatment. New York: Oxford University Press.
- Kramer, Peter D (2005). Against Depression. New York: Viking Adult
- Weissman, M. M., Markowitz, J. C., & Klerman, G. L. (2000). Comprehensive guide to interpersonal psychotherapy. New York: Basic Books.
- Sarbadhikari S. N. (2005).Ed, Depression and Dementia:Progress in Brain Research, Clinical Applications and Future Trends. Hauppauge, Nova Science Publishers. [24] ISBN 1-59454-114-0
Books by persons suffering or having suffered from depression
- Wurtzel, E. (1997) Prozac Nation: Young and Depressed in America: A Memoir. Riverhead Books. ISBN 1573225126
- Lewinsohn, P. M., Munoz, R. F, Youngren, M. A., Zeiss, A. M. (1992). Control your depression. New York: Fireside/Simon&Schuster.
- Nesaule,
Agate (1995). A Woman in Amber: Healing the Trauma of War and
Exile New York: Penguin Books.
- ISBN 1-56947-046-4 (hc.); 0 14 02.6190 7 (pbk.)
- Rowe, Dorothy (2003). Depression: The way out of your prison. London: Brunner-Routledge.
- Sealey, Robert (2002). Finding Care for Depression, Mental Episodes & Brain Disorders, Toronto: Sear Publications www.searpubl.ca
- Shields, Brooke (2005). Down Came the Rain: My Journey Through Postpartum Depression. Hyperion. ISBN 1401301894.
- Smith, Jeffery (2001). Where the roots reach for water: A personal and natural history of melancholia. New York: North Point Press.
- Solomon, Andrew (2001). The noonday demon: An atlas of depression. New York: Scribner.
- Styron, William (1992). Darkness visible: A memoir of madness. New York: Vintage Books/Random House.
- Wolpert, Lewis (2001). Malignant sadness: The anatomy of depression. London: Faber and Faber.
- Tolle, Eckhart (1999). The Power of Now: A Guide to Spiritual Enlightenment, New World Library, October, 1999 ISBN 1577311523 (HC) ISBN 1577314808 (PB)
Sources
- ^ Schildkraut, J.J. (1965). "The catecholamine hypothesis of affective disorders: a review of supporting evidence". Am J Psychiatry 122 (5): 509-22.
- ^ Hirschfeld, R.M.A (2000). "History and Evolution of the Monoamine Hypothesis of Depression". J Clin Psychiatry 61 (Suppl. 6): 4-6.
- ^ Bland, R.C. (1997). "Epidemiology of Affective Disorders: A Review". Can J Psychiatry 42: 367–377.
- ^ Murray, C.J.L., Lopez, A.D. (1997). "Alternative projections of mortality and disability by cause 1990-2020: Global Burden of Disease Study". Lancet 349: 1498–1504.
- ^ Manev, R, Manev H (2004). "5-Lipoxygenase as a putative link between cardiovascular and psychiatric disorders". Critical Reviews in Neurobiology 16 (1–2): 181–6.
- ^ Lawrence, Felicity (2004). "The Ready Meal" Kate Barker Not on the Label, 214, Penguin. ISBN 0-141-01566-7.
- ^ Using Fatty Acids for Enhancing Classroom Achievement. URL accessed on January, 2004.
- ^ Delle Chiaie, Roberto, Paolo Pancheri and Pierluigi Scapicchio (2002). "Efficacy and tolerability of oral and intramuscular S-adenosyl- L-methionine 1,4-butanedisulfonate (SAMe) in the treatment of major depression: comparison with imipramine in 2 multicenter studies". Am J Clin Nutr 76 (5): 1172S–1176S.
- ^ Mischoulon, D, Fava M. (2002). "Role of S-adenosyl-L-methionine in the treatment of depression: a review of the evidence". Am J Clin Nutr 76 (5): 1158S–61S.
- ^ Keller, M.B. (2003). "Past, Present, and Future Directions for Defining Optimal Treatment Outcome in Depression". JAMA 289: 3152–3160.
- ^ Martin, JL, Barbanoj MJ, Schlaepfer TE, Thompson E, Perez V, Kulisevsky J (June 2003). "Repetitive transcranial magnetic stimulation for the treatment of depression. Systematic review and meta-analysis". British Journal of Psychiatry 182: 480-91. PMID 12777338.
- ^ Geddes, JR, Carney SM, Davies C, Furukawa TA, Kupfer DJ, Frank E, Goodwin GM (22 February 2003). "Relapse prevention with antidepressant drug treatment in depressive disorders: a systematic review". Lancet 361 (9358): 653–61. PMID 12606176.
External links
- National Institute of Mental Health - Depression booklet
- Depression at the Open Directory Project